A nurse is preparing to auscultate a client’s heart, a crucial procedure that requires careful preparation and skilled technique. This comprehensive guide will delve into the essential steps and considerations involved in auscultation, empowering nurses with the knowledge and expertise to perform accurate and informative heart sound assessments.
Auscultation, the act of listening to sounds produced by the body, plays a vital role in cardiac assessment. By placing a stethoscope on the chest, nurses can detect and interpret heart sounds, providing valuable insights into the heart’s function and overall health.
Pre-Auscultation Preparation

Auscultation is a vital part of physical assessment, providing valuable information about the heart’s function. Proper preparation is crucial for accurate and effective auscultation.
Hand Hygiene and PPE
- Perform thorough hand hygiene before and after auscultation to prevent the spread of infection.
- Wear appropriate personal protective equipment (PPE), such as gloves, to protect yourself from potential bloodborne pathogens.
Client Positioning
- Position the client in a comfortable, semi-Fowler’s position or sitting upright with their back supported.
- Expose the client’s chest adequately, ensuring the skin is clean and dry.
- Instruct the client to breathe deeply and regularly through their nose.
Calm and Quiet Environment
Creating a calm and quiet environment is essential for accurate auscultation. Minimize distractions and background noise to enhance sound transmission and perception.
Auscultation Technique
Correct stethoscope placement and technique are crucial for optimal heart sound detection.
Stethoscope Placement
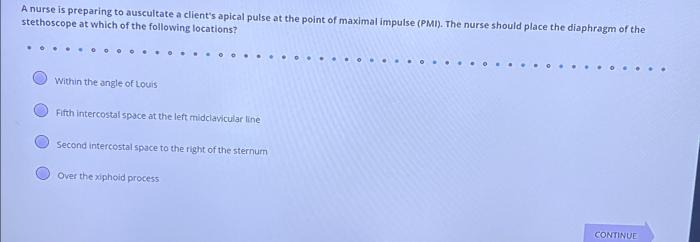
- Place the diaphragm of the stethoscope directly over the apex of the heart (5th intercostal space, midclavicular line) for the best transmission of high-pitched sounds.
- Use the bell for low-pitched sounds, such as murmurs, gallops, or pericardial rubs.
Heart Valve Areas
- Aortic area:2nd right intercostal space, sternal border
- Pulmonary area:2nd left intercostal space, sternal border
- Tricuspid area:5th left intercostal space, left sternal border
- Mitral area:5th intercostal space, midclavicular line
Diaphragm vs. Bell, A nurse is preparing to auscultate a client’s heart
- The diaphragm is used for high-pitched sounds (S1, S2) due to its greater sensitivity.
- The bell is used for low-pitched sounds (murmurs, gallops) due to its ability to amplify lower frequencies.
Heart Sound Interpretation

Normal and abnormal heart sounds provide important clues about cardiac function.
Normal Heart Sounds
- S1:Closing of the mitral and tricuspid valves (lubb)
- S2:Closing of the aortic and pulmonary valves (dupp)
Abnormal Heart Sounds
- Murmurs:Swishing or blowing sounds caused by turbulent blood flow
- Gallops:Extra heart sounds that resemble a horse’s gallop
- Clicks:Short, high-pitched sounds associated with valve abnormalities
Heart Sound Variations
Variations in heart sounds can indicate underlying cardiac conditions, such as:
- Increased S1: Mitral stenosis
- Diminished S2: Aortic or pulmonary stenosis
- Split S2: Bundle branch block
Documentation and Communication
Accurate documentation and communication of auscultation findings are essential for patient care.
Documentation
- Document the location and characteristics of all heart sounds heard.
- Include any abnormal sounds or variations noted.
- Use standardized terminology and reporting formats.
Communication
- Effectively communicate auscultation findings to other healthcare professionals.
- Provide a clear and concise description of heart sounds and any abnormalities detected.
- Discuss the clinical significance and implications of auscultation findings.
Special Considerations: A Nurse Is Preparing To Auscultate A Client’s Heart
Certain factors may affect heart sound transmission and require special considerations.
Obesity
- Excess adipose tissue can dampen heart sounds, making auscultation more challenging.
- Use a larger diaphragm and apply more pressure to enhance sound transmission.
Pulmonary Conditions
- Conditions such as emphysema or pneumonia can alter lung sounds, affecting heart sound transmission.
- Consider using alternative auscultation techniques, such as apex-axillary or Erb’s point.
Ongoing Assessment
Regular auscultation is essential for monitoring heart sounds in clients with known cardiac conditions.
- Track changes in heart sounds over time to identify potential complications or disease progression.
- Refer clients for further evaluation if significant changes or new abnormal sounds are detected.
Answers to Common Questions
What is the importance of proper hand hygiene before auscultation?
Hand hygiene helps prevent the transmission of microorganisms and ensures patient safety during auscultation.
How should the client be positioned for optimal auscultation?
The client should be positioned in a comfortable, upright or semi-recumbent position, with the chest exposed.
What is the difference between using the diaphragm and bell of the stethoscope?
The diaphragm is used for high-pitched sounds, while the bell is used for low-pitched sounds.
What are some examples of abnormal heart sounds?
Abnormal heart sounds include murmurs, gallops, and clicks, which may indicate underlying cardiac conditions.